Dr. Richard Nagelberg--a dentist with over 30 years of experience--has been featured quite a few times recently on Dentistry IQ. The topic of his choice? Periodontal disease. Nagelberg gently calls out other dentists and their efforts in treating this disease. Is he on to something, or is he off the mark?
He may have a point. If you think back to your previous dental cleanings, do you remember anyone discussing periodontal disease with you? Unless it's already an issue, probably not. After all, why should patients with healthy teeth and gums be worried about something they don't have? The problem is that this lack of concern, or education, among patients means that some dentist offices are missing the preventative aspect. Obviously if a patient develops periodontal disease, he or she will be treated accordingly. But Dr. Nagelberg argues that dentists could be doing so much more.
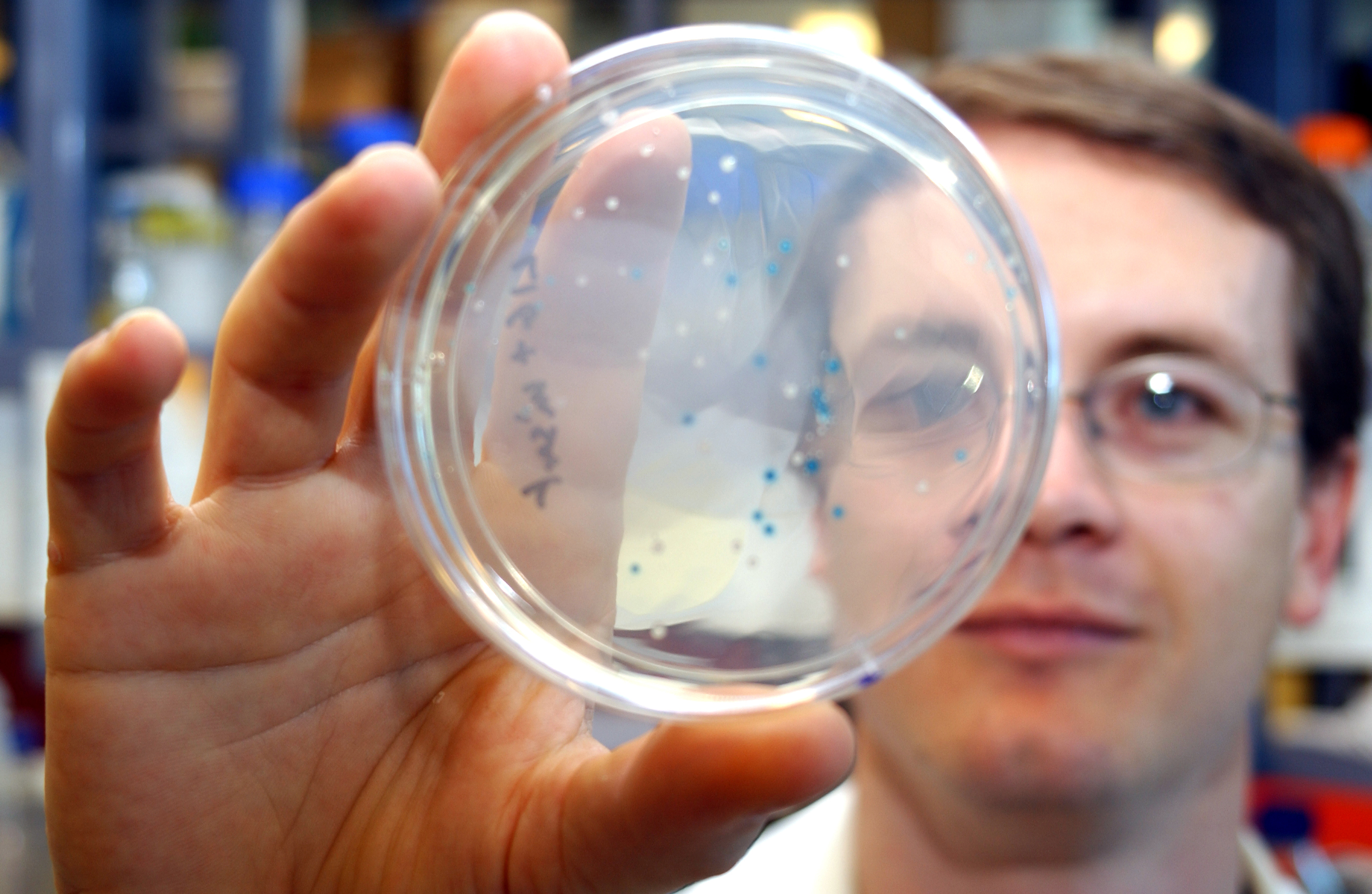
Periodontal disease is often measured by probing gum pockets and assessing the inflammation of the gums. However, dentists could go a step further and address not only the signs of disease, but the source: the bacteria in the gums. Take a look:
Bacterial ID for prevention of periodontal disease
The hallmark of prevention is to identify risk factors for disease and then to manage those risk factors before the disease, condition, or event occurs. This is why there is so much information available regarding the risk factors for cardiovascular disease. Periodontal disease is no exception. Identify the biggest risk factor for periodontal disease—namely, the specific bacteria a patient harbors in his or her mouth—and then manage it with an antimicrobial protocol before periodontal disease rears its ugly head.
Patients who have a strong family history of periodontal disease would be an ideal place to start. Since you can reasonably predict that these individuals have some level of elevated risk for periodontal disease, why not find out which oral bacteria they have? And the same for patients with gingivitis who have not yet progressed to periodontitis. If the test shows very few bacteria at low levels, we can conclude that, at this time, the patient is not at risk for the development of periodontal disease, and vice versa. This just makes sense.
Maybe the reason more bacterial IDing doesn't occur is because patients want to get in and out of the office as quickly as possible. Or maybe it's because dentists are just used to looking at signs that can be observed in office since the molecular technology used to identify bacteria is relatively recent in the medical world.
Today, DNA-PCR testing (a lab technique that can make copies of a DNA section) can be used to identify the specific bacteria causing periodontal disease before symptoms appear! And this testing is severely underutitlized--especially since it is so easy to do. As a patient, you just need to get your cheek swabbed or spit in a cup, and then that sample is analyzed in a lab. Even though there are over 600 million kinds of bacteria in your mouth, this test is able to identify the most common bacteria--like P. gingivalis, E. nodatum, A. actinomyceemcomitans--which cause the disease.
Since early periodontal disease is easily treated and there are more than 3 million cases (according to the Mayo clinic), early preventative methods should be a must for everyone.
If patients want to forgo testing, they should at least be aware of the secondary conditions that can develop with periodontal disease. The Dental Tribune just released a short sampling of different studies that illustrate the correlation:
Alzheimer’s, cognitive decline linked to periodontal disease
Recent studies provide increasing evidence that untreated periodontal inflammation is linked to cognitive decline and Alzheimer’s disease, and that treating periodontitis may reduce or delay risk of this disease. About one out of every nine Americans have some form of Alzheimer’s disease, according to the Alzheimer’s Society. It is the worst type of dementia, involving the most cognitive decline and memory loss.
Research has already found Porphyromonas gingivalis (P. gingivalis) in brains of Alzheimer’s patients. P. gingivalis is a bacterium associated with chronic periodontitis. Researchers propose that when these bacteria reach the brain, an immune response is stimulated in the brain to release proteins that kill the bacteria, but also cause broader destruction . . .
A study by professor Stjohn Crean and Dr. Sim Singhrao at the University of Central Lancashire (UCLan) School of Medicine and Dentistry in England involved the examination of brain tissue samples of 10 deceased people with Alzheimer’s and 10 people without it.
It was found that bacteria found in chronic periodontal disease were present in the brains of four of the 10 people with Alzheimer’s but in none of the 10 without it. Researchers theorized that chronic periodontal disease bacteria, P. gingivalis, enter the bloodstream and brain, prompting an immune system response, which over time is thought to contribute to cognitive decline and Alzheimer’s disease.
Along with Alzheimer's, there's many studies that show a link between periodontal disease and issues like heart disease, respiratory diseases, autoimmune diseases, diabetes, and so on. If a quick swab of your cheeks can help you prevent not only periodontal disease but other serious conditions, why not go for it?
The post Testing for Periodontal Disease is Easier Than Ever appeared first on Dental Oasis Of Orange County.
Dental Oasis Of Orange County
7777 Edinger Ave #232
Huntington Beach, CA 92647
(714) 894-7700
drtoorani@dentaloasisofoc.com
Google My Business Listing
Google Map
Directions to our office
Yelp Page
No comments:
Post a Comment